Diuretics |
please flag with care:
| |
| 2008-11-01 | No history |  | Add My version | |
download mind map 145600728.mmap (mindmap file created by MindManager)
| | |
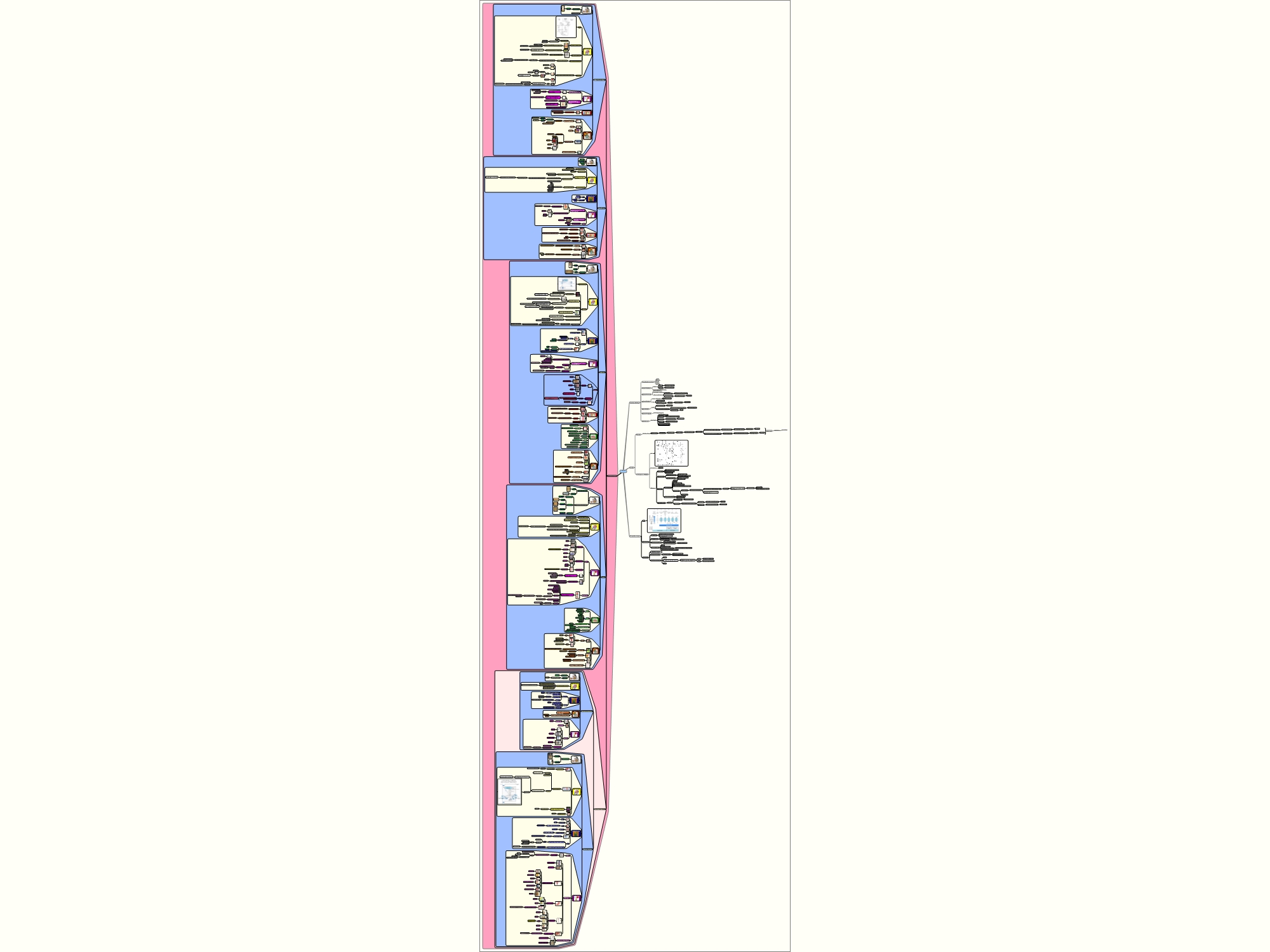
| I am currently studying for a post graduate degree in pharmacology and this is one of my maps to try to get all the info into my head. They do not conform to traditional mindmap standards but I am trying to visualize everything as far as possible. Therefore the maps are quiet large. Diuretic one is 2.48MB at this stage and to date only about 80% complete. | |
 | |
| outline | |
Diuretics
-------------------------------------------------------------
1 Functions of the Kidney
-------------------------------------------------------------
1.1 Regulates blood ionic concentrates
1.1.1 sodium
1.1.2 potassium
1.1.3 calcium
1.1.4 chloride
1.1.5 phosphates
1.2 monitors blood osmolarity
1.2.1 difference
1.2.1.1 osmolarity
1.2.1.1.1 number of particles per litre
1.2.1.2 osmolality
1.2.1.2.1 number of particles per kg
1.2.2 terms are interchangeable in physiology
1.3 regulation of blood volume
1.3.1 blood volume affects BP
1.3.2 changing interstitual volume gives rise to oedema
1.3.3 kidneys also secrete renin
1.3.3.1 renin effects the RAAS
1.3.3.1.1 RAAS important in BP and salt control
1.3.3.2 renin is a vasoconstrictor
1.3.3.2.1 increased renal resistance
1.3.3.2.1.1 increased BP
1.4 regulation of blood pH
1.4.1 if you want to change pH
1.4.1.1 change H+ concentration
1.4.2 kidney
1.4.2.1 increased H+ excretion
1.4.2.2 increased HCO3 resorption
1.4.2.2.1 bicarbonate
1.4.2.2.1.1 maintains acid balance
1.4.2.2.1.1.1 acts as a buffer
1.5 regulates hormones
1.5.1 Calcitrol
1.5.1.1 active form of vitamin D
1.5.1.1.1 stored in kidney
1.5.1.2 main function is calcium metabolism
1.5.1.2.1 stimulates calcium binding protein synthesis
1.5.1.2.1.1 increases calcium uptake
1.5.1.2.2 difficiency in calcium
1.5.1.2.2.1 ricketts
1.6 regulation of blood glucose
1.6.1 controls resorpsion of glucose
1.7 excretion of wastes
1.7.1 by forming urine
1.7.1.1 puts urea and NH4 in urine
1.7.1.2 adds bilirubin
1.7.1.2.1 formed from breakdown of haemoglobin
1.7.1.3 adds creatine
1.7.1.3.1 from breakdown of muscle
1.7.1.3.1.1 creatinephosphate
1.7.1.4 adds uric acid
1.7.1.4.1 from breakdown of nucleic acids
1.7.1.5 elimination of drugs and toxins
-------------------------------------------------------------
2 Anatomy
-------------------------------------------------------------
2.1 blood supply
2.1.1 main renal artery
2.1.1.1 interlobar arteries
2.1.1.1.1 arcuate arteries
2.1.1.1.1.1 interlobular arteries
2.1.1.1.1.1.1 afferent arterioles
2.1.1.1.1.1.1.1 glomerular capillary nexus
2.1.1.1.1.1.1.1.1 efferent arterioles
2.1.1.1.1.1.1.1.1.1 efferent arterioles of the superficial glomeruli
2.1.1.1.1.1.1.1.1.1.1 ascend to the kidney surface
2.1.1.1.1.1.1.1.1.1.1.1 split into peritubular capillaries
2.1.1.1.1.1.1.1.1.1.1.1.1 interlobular veins
2.1.1.1.1.1.1.1.1.1.1.1.1.1 arcuate veins
2.1.1.1.1.1.1.1.1.2 efferent arterioles of the juxtamedullary glomeruli
2.1.1.1.1.1.1.1.1.2.1 descend into the medulla
2.1.1.1.1.1.1.1.1.2.1.1 divide to form the descending vasa recta
2.1.1.1.1.1.1.1.1.2.1.1.1 ascending vasa recta
2.1.1.1.1.1.1.1.1.2.1.1.1.1 arcuate veins
2.1.1.1.1.1.1.1.1.1 interlobular veins
2.1.1.1.1.1.1.1.1.1.1 segmental veins
2.1.1.1.1.1.1.1.1.1.1.1 main renal vein
2.2 functional apparatus is the nephron
2.2.1 figure
2.2.1.1
2.2.2 filtering apparatus
2.2.2.1 glumerulus
2.2.3 tubular portion
2.2.3.1 proximal tubule
2.2.3.1.1 65% of filtered sodium reabsorbed here
2.2.3.1.2 highly permeable to water
2.2.3.1.3 reabsorbsion isotonic
2.2.3.2 intermediate tubule
2.2.3.2.1 descending thin limb (DTL)
2.2.3.2.1.1 highly permeable to water
2.2.3.2.1.2 low permeability to sodium and urea
2.2.3.2.2 ascending thin limb (ATL)
2.2.3.2.2.1 permeable to sodium and urea
2.2.3.2.2.2 impermeable to water
2.2.3.3 distal tubule
2.2.3.3.1 thick ascending limb
2.2.3.3.1.1 in medulla
2.2.3.3.1.2 in cortex
2.2.3.3.1.3 actively reabsorbs NaCl
2.2.3.3.1.4 impermeable to urea and water
2.2.3.3.1.5 25% of filtered sodium reabsorbed in loop of Henle
2.2.3.3.1.6 passes between
2.2.3.3.1.6.1 afferent arterioles
2.2.3.3.1.6.1.1 makes contact with macula densa
2.2.3.3.1.6.1.1.1 senses concentration of NaCl leaving loop of Henle
2.2.3.3.1.6.1.1.1.1 if [NaCl] is high
2.2.3.3.1.6.1.1.1.1.1 send chemical signal to afferent arteriole of same nephron
2.2.3.3.1.6.1.1.1.1.1.1 causing it to constrict
2.2.3.3.1.6.1.1.1.1.1.1.1 decreases GFR
2.2.3.3.1.6.1.1.1.1.1.1.2 known as tubuloglomerular feedback
2.2.3.3.1.6.1.1.2 also regulates renin release from adjacent juxtaglomerular cells
2.2.3.3.1.6.2 efferent arterioles
2.2.3.3.2 distal convoluted tubule (DCT)
2.2.3.3.2.1 actively transports NaCl
2.2.3.3.2.2 impermeable to water
2.2.3.4 collecting duct system
2.2.3.4.1 in control of
2.2.3.4.1.1 ultrafiltrate composition
2.2.3.4.1.1.1 modulated by aldosterone
2.2.3.4.1.2 volume of urine
2.2.3.4.1.2.1 modulated by antidiuretic hormone (ADH)
2.2.3.4.1.2.1.1 absence of ADH
2.2.3.4.1.2.1.1.1 collecting duct impermeable to water
2.2.3.4.1.2.1.1.1.1 diluted urine
2.2.3.4.1.2.1.2 presence of ADH
2.2.3.4.1.2.1.2.1 collecting duct permeable to water
2.2.3.4.1.2.1.2.1.1 concentrates urine
-------------------------------------------------------------
3 Renal epithelial transport
-------------------------------------------------------------
3.1 figure
3.1.1
3.2 Passive transport
3.2.1 Solvent drag
3.2.1.1 during bulk water flow across a membrane
3.2.1.2 solvent molecules will be transferred across the membrane
3.2.2 Simple diffusion
3.2.2.1 lipid soluble solutes may dissolve in membrane
3.2.2.2 diffuse across membrane
3.2.2.2.1 down their electrochemical gradient
3.2.3 Channel-mediated diffusion
3.2.3.1 solutes with limited lipid solubility
3.2.3.2 diffuse passively through "pores"
3.2.3.2.1 formed by integral proteins
3.2.4 Facilitated diffusion
3.2.4.1 Uniport
3.2.4.2 carrier mediated diffusion
3.2.4.3 Solute may bind to integral protein
3.2.4.3.1 and owing to a conformational change in protein
3.2.4.4 be transported down an electrochemical gradient
3.3 Active transport
3.3.1 movement of solute against electrochemical gradient
3.3.2 primary active transport
3.3.2.1 ATP-mediated transport
3.3.2.1.1 ATP hydrolysis is coupled to
3.3.2.1.2 conformational changes in integral proteien
3.3.3 secondary active transport
3.3.3.1 Symport
3.3.3.2 ATP-mediated transport used to create an electrochemical gradient for one solute
3.3.3.2.1 "free energy"of that solute is then used for the "uphill" transport of other solutes
3.3.3.2.1.1 symport
3.3.3.2.1.1.1 co-transport in same direction
3.3.3.2.1.2 antiport
3.3.3.2.1.2.1 co-transport in opposite direction
3.3.3.3 Antiport
-------------------------------------------------------------
4 Principles of diuretic action
-------------------------------------------------------------
4.1 Carbonic Anhydrase Inhibitors
4.1.1 Examples
4.1.1.1 Acetazolamide
4.1.1.1.1 Diamox
4.1.1.1.1.1
4.1.1.2 limited use as diuretics
4.1.2 Mode of Action
4.1.2.1 figure
4.1.2.1.1
4.1.2.2 proximal tubular epithelial cells
4.1.2.2.1 carbonic anhydrase
4.1.2.2.1.1 enzyme
4.1.2.2.1.2 plays key role in NaHCO3
4.1.2.2.1.2.1 reabsorbtion
4.1.2.2.1.2.2 acid secretion
4.1.2.2.2
4.1.2.2.2.1 net effect is to move NaHCO3 from the tubular lumen
4.1.2.2.2.1.1 to the interstitial space
4.1.2.2.2.1.2 followed by the movement of water
4.1.2.2.2.1.2.1 isotonic reabsorbtion
4.1.2.2.3
4.1.2.2.3.1 removal of water concentrates Cl- in the lumen
4.1.2.2.3.1.1 Cl- diffuses down its concentration gradient into interstitium
4.1.2.2.3.1.1.1 via paracellular pathway
4.1.2.3 effects on urinary excretion
4.1.2.3.1
4.1.2.3.1.1 nett effect due to a few mechanisms
4.1.2.3.1.1.1 loss of bicarbonate-, potassium ions and water
4.1.2.4 effects on renal haemodynamics
4.1.2.4.1 inhibits proximal reabsorbtion
4.1.2.4.1.1 increased delivery of solutes to macula densa
4.1.2.4.1.1.1 triggers TGF system
4.1.2.4.1.1.1.1 increased afferent arteriole resistance
4.1.2.4.1.1.1.1.1 reduced renal blood flow
4.1.2.4.1.1.1.1.2 reduced glomerular filtration rate
4.1.2.5 other actions
4.1.2.5.1 carbonic anhydrase (CA) in numerous other tissues
4.1.2.5.1.1
4.1.2.5.1.1.1 gastric mucosa
4.1.2.5.1.2
4.1.2.5.1.2.1 pancreas
4.1.2.5.1.3
4.1.2.5.1.3.1 CNS
4.1.2.5.1.3.1.1 can cause
4.1.2.5.1.3.1.1.1 parasthesias
4.1.2.5.1.3.1.1.2
4.1.2.5.1.3.1.1.2.1 somnolence
4.1.2.5.1.3.1.2
4.1.2.5.1.3.1.2.1 used in epilepsy
4.1.2.5.1.3.1.2.1.1 due to metabolic acidosis effect of asetazolamide
4.1.2.5.1.4
4.1.2.5.1.4.1 erythrocytes
4.1.2.5.1.5
4.1.2.5.1.5.1 eye
4.1.2.5.1.5.1.1 CA mediates the formation of large amounts of bicarbonate ions in
4.1.2.5.1.5.1.1.1 cilliary process of the eye
4.1.2.5.1.5.1.1.2 inhibition of CA
4.1.2.5.1.5.1.1.2.1 decreases rate of formation of aqueous humour
4.1.2.5.1.5.1.1.2.1.1 reduced ocular pressure
4.1.3 Adverse effects
4.1.3.1 is a sulphonamide derivate
4.1.3.1.1
4.1.3.1.1.1 patients hypersensitive to sulphonamides
4.1.3.1.1.1.1 can cause
4.1.3.1.1.1.1.1 bone marrow depletion
4.1.3.1.1.1.1.2 skin toxicity
4.1.3.1.1.1.1.3 allergic reactions
4.1.3.2 most are due to urine alkalisation and metabolic acidosis
4.1.3.2.1
4.1.3.2.1.1 diversion of ammonia of renal origin from urine to systemic circulation
4.1.3.2.1.1.1 can worsen hepatic encephalopathy
4.1.3.2.2 alkaline urine
4.1.3.2.2.1 calculus formation and urethral colic
4.1.3.2.3
4.1.3.2.3.1 worsening of metabolic or respiratory acidosis
4.1.3.2.4 reduction of urinary excretion of weak basis
4.1.4 Contra-indications
4.1.4.1
4.1.4.1.1 patients with chirrhosis
4.1.4.1.1.1 may cause hyperammonemia
4.1.4.1.1.2 hepatic encephalopathy
4.1.5 Uses
4.1.5.1
4.1.5.1.1 open-angle glaucoma
4.1.5.1.1.1 topical compound
4.1.5.1.1.1.1 Dorzolamide
4.1.5.1.1.1.1.1 Trusopt
4.1.5.1.1.1.1.1.1 single ingredient
4.1.5.1.1.1.1.2 Cosopt
4.1.5.1.1.1.1.2.1 multi ingredient
4.1.5.1.1.1.2 no diuretic effect
4.1.5.1.1.1.3 no systemic metabolic effects
4.1.5.2
4.1.5.2.1 oedema
4.1.5.3
4.1.5.3.1 epilepsy
4.1.5.4
4.1.5.4.1 altitude sickness
4.1.5.4.1.1 symptomatic relief
4.1.5.4.1.1.1 give prophylactic
4.1.5.4.1.2 symptoms
4.1.5.4.1.2.1 weakness
4.1.5.4.1.2.2 dizziness
4.1.5.4.1.2.3
4.1.5.4.1.2.3.1 insomnia
4.1.5.4.1.2.4
4.1.5.4.1.2.4.1 headache
4.1.5.4.1.2.5
4.1.5.4.1.2.5.1 nausea
4.1.5.5
4.1.5.5.1 to correct metabolic alkalosis
4.2 Osmotic Diuretics
4.2.1 Examples
4.2.1.1 glycerin
4.2.1.2 isosorbide
4.2.1.3 mannitol
4.2.1.4 urea
4.2.2 Mode of Action
4.2.2.1 freely filtered by glomerulus
4.2.2.1.1 limited reabsorbtion
4.2.2.1.2 relatively inert pharmacologically
4.2.2.2 primary site of action
4.2.2.2.1 loop of Henle
4.2.2.3 extract water from intracellular compartments
4.2.2.3.1 therefore expand extracellular fluid volume
4.2.2.3.1.1 decrease blood viscosity
4.2.2.3.1.2 inhibit renin release
4.2.2.3.2 these effects increase RBF
4.2.2.3.2.1 increase in renal medullary blood flow
4.2.2.3.2.1.1 removes NaCl and urea from the renal medulla
4.2.2.3.2.1.1.1 reduces medullary tonicity
4.2.2.3.2.1.1.1.1 decrease in extraction of water from the DTL
4.2.2.3.2.1.1.1.1.1 limits the [NaCl] in the tubular fluid entering the ATL
4.2.2.3.2.2 prostaglandins can have same effect
4.2.2.4 effects on urinary excretion
4.2.2.4.1 increase urinary excretion of
4.2.2.4.1.1 nearly all electolytes
4.2.2.4.1.1.1 Na
4.2.2.4.1.1.2 K
4.2.2.4.1.1.3 Calcium
4.2.2.4.1.1.4 Magnesium
4.2.2.4.1.1.5 Chloride
4.2.2.4.1.1.6 bicarbonate
4.2.2.4.1.1.7 phosphate
4.2.3 Pharmacokinetics
4.2.3.1 oral
4.2.3.1.1 glycerine
4.2.3.1.2 isosorbide
4.2.3.2 parenteral (IV)
4.2.3.2.1 mannitol
4.2.3.2.2 urea
4.2.4 Adverse effects
4.2.4.1 mostly due to extracellular fluid volume expansion
4.2.4.1.1
4.2.4.1.1.1 heart failure patients
4.2.4.1.1.1.1 contraindicated
4.2.4.1.1.1.1.1 pulmonary edema
4.2.4.1.2 can cause hyponatremia in cells
4.2.4.1.2.1
4.2.4.1.2.1.1 headache
4.2.4.1.2.2
4.2.4.1.2.2.1 nausea
4.2.4.1.2.2.2 vomiting
4.2.4.2 loss of water in excess of electrolytes
4.2.4.2.1 hypernatremia
4.2.4.2.2
4.2.4.2.2.1 dehydration
4.2.4.3 urea
4.2.4.3.1 with extravasation
4.2.4.3.1.1 thrombosis
4.2.4.3.1.2 pain
4.2.5 Contra-indications
4.2.5.1
4.2.5.1.1 severe renal disease
4.2.5.1.1.1 not in anuric patients
4.2.5.2
4.2.5.2.1 impaired liver function
4.2.5.2.1.1 do not give urea
4.2.5.2.1.1.1 can lead to elevation of blood ammonia levels
4.2.5.3
4.2.5.3.1 active cranial bleeding
4.2.5.3.1.1 urea
4.2.5.3.1.2 mannitol
4.2.5.4 glycerin
4.2.5.4.1 is metabolised
4.2.5.4.1.1 can cause hyperglycemia in diabetics
4.2.6 Uses
4.2.6.1
4.2.6.1.1 glaucoma
4.2.6.1.1.1 by increasing the osmotic pressure of the plasma
4.2.6.1.1.1.1 exctracs water from the eye and brain
4.2.6.2
4.2.6.2.1 eye surgery
4.2.6.2.1.1 to reduce intra-ocular pressure
4.2.6.3
4.2.6.3.1 neurosurgery
4.2.6.3.1.1 to reduce brain mass and cerebral edema
4.2.6.3.1.1.1 pre- and post operativly
4.2.6.3.1.1.1.1 mannitol
4.2.6.3.1.1.1.2 urea
4.3 Loop Diuretics
4.3.1 Examples
4.3.1.1 Furosemide
4.3.1.1.1 Lasix
4.3.1.1.1.1
4.3.1.1.2 Puresis
4.3.1.2 Torasemide
4.3.1.2.1 Utin
4.3.1.2.1.1
4.3.2 Mode of Action
4.3.2.1 figure of normal action
4.3.2.1.1
4.3.2.2 Site of action
4.3.2.2.1
4.3.2.2.1.1 Thick ascending limb
4.3.2.2.1.1.1 inhibitors of Na+-K+-2Cl-Symport
4.3.2.2.1.1.2 symporter captures free energy in the sodium electrochemical gradient established
4.3.2.2.1.1.2.1 provides energy for uphill transport of potassium and chloride into the cell
4.3.2.2.2 diuretics inhibit symporter for sodium,potassium and chloride
4.3.2.2.2.1
4.3.2.2.2.1.1 reduce the reabsorbtion of NaCl
4.3.2.2.2.1.1.1 up to 25% of filtered sodium excreted by these diuretics
4.3.2.2.2.2 also diminish the positive potential that comes from K+ recycling
4.3.2.2.2.2.1 positive potential drives divalent cation reabsorbtion
4.3.2.2.2.2.2 therfore magnesium and calcium excretion is increased by loop diuretics
4.3.2.2.2.2.2.1 prolonged use can cause hypomagnesia
4.3.2.2.3 induce synthesis of renal prostaglandins
4.3.2.2.3.1 effects on blood vessel
4.3.2.2.3.1.1 NSAIDS can inhibit this formation
4.3.2.2.3.1.1.1 effect is worse in patients with nephrotic syndrome and hepatic cirrhosis
4.3.2.2.3.1.2 loop diuretics increase renal blood flow
4.3.2.2.4
4.3.2.2.4.1 loop diuretics block the kidneys abillity to concentrate the urine during hydropenia
4.3.2.2.5 are powerful stimulators of renin release
4.3.2.2.5.1 due to interference of NaCl transport by the macula densa
4.3.2.2.6 increase systemic venous capacitance
4.3.2.2.6.1 decrease left ventricular filling rate
4.3.2.2.6.1.1 especially furosemide
4.3.2.2.6.1.2 benefits patients with pulmonary edema
4.3.2.2.7 chronic administration
4.3.2.2.7.1 increased uric acid levels
4.3.2.2.7.1.1 due to
4.3.2.2.7.1.1.1 increased reabsorbtion of uric acid
4.3.2.2.7.1.1.2 competition between diuretic and uric acid
4.3.2.2.7.1.1.2.1 for organic acid secretion in proximal tubule
4.3.2.2.7.1.1.2.1.1 reduced uric acid secretion
4.3.3 Pharmacokinetics
4.3.3.1 are rapidly absorbed
4.3.3.2
4.3.3.2.1 highly bound to proteins
4.3.3.3 eliminated
4.3.3.3.1
4.3.3.3.1.1 kidneys
4.3.3.3.1.1.1 glomerular filtration
4.3.3.3.1.1.2 tubular secretion
4.3.3.3.1.1.3 reduction of secretion by
4.3.3.3.1.1.3.1 NSAIDs
4.3.3.3.1.1.3.2 Probenecid
4.3.3.3.2
4.3.3.3.2.1 short elimination half-life
4.3.3.3.3
4.3.3.3.3.1 two drugs mentioned - liver as well
4.3.3.3.3.1.1 Torasemide
4.3.3.3.3.1.1.1 Utin
4.3.3.3.3.1.2 Bumetanide
4.3.3.3.3.1.2.1 Burinex
4.3.3.3.3.1.3 elimination of above prolonged by liver disease
4.3.4 Adverse effects
4.3.4.1 due to abnormalities of fluid and electrolyte balance
4.3.4.1.1 extra cellular fluid volume depletion
4.3.4.1.1.1
4.3.4.1.1.1.1 hypotension
4.3.4.1.1.2 reduced GFR
4.3.4.1.1.3 circulatory collapse
4.3.4.1.1.4 thromboembolic episodes
4.3.4.1.1.5 patients with liver disease
4.3.4.1.1.5.1 hepatic encephalopathy
4.3.4.1.2 hyponatremia
4.3.4.1.3
4.3.4.1.3.1 hypokalemia
4.3.4.1.3.1.1 if dietary intake of potassium not sufficient
4.3.4.1.3.1.2 can cause
4.3.4.1.3.1.2.1 cardiac arrhythmias
4.3.4.1.4 hypomagnesia
4.3.4.1.4.1 due to incresed excretion of magnesium
4.3.4.1.4.1.1 risk factor in cardiac arrhthmias
4.3.5 Toxicity
4.3.5.1
4.3.5.1.1 ototoxicity
4.3.5.1.1.1
4.3.5.1.1.1.1 tinnitus
4.3.5.1.1.2
4.3.5.1.1.2.1 hearing impairment
4.3.5.1.1.3
4.3.5.1.1.3.1 deafness
4.3.5.1.1.4
4.3.5.1.1.4.1 vertigo
4.3.5.1.1.5
4.3.5.1.1.5.1 mostly with rapid intravenous administration
4.3.5.2 hypochloremic alkalosis
4.3.5.2.1 caused by
4.3.5.2.1.1 due to increased sodium delivery to distal tubule
4.3.5.2.1.2 combined with activation of the RAS
4.3.5.2.1.1 leads to increased urinary excretion of potassium and hydrogen ions
4.3.5.3
4.3.5.3.1 gout patients
4.3.5.3.1.1 hyperuricemia
4.3.5.3.1.1.1 can lead to gout
4.3.6 Contra-indications
4.3.6.1
4.3.6.1.1 postmenopausal woman
4.3.6.1.1.1 calcium excretion bad for bone metabolism
4.3.6.2
4.3.6.2.1 diabetic patients
4.3.6.2.1.1 hypoglycemia
4.3.6.2.1.1.1 can be caused by loop diuretics
4.3.6.3
4.3.6.3.1 cholesterol
4.3.6.3.1.1 can increase plasma levels of LDL
4.3.6.3.1.1.1 decreases HDL levels
4.3.6.4 hypersensitivity to sulfonamides
4.3.7 Interactions
4.3.7.1 Aminoglycosides
4.3.7.1.1 synergism of ototoxicity
4.3.7.2
4.3.7.2.1 anticoagulants
4.3.7.2.1.1 increased anticoagulant activity
4.3.7.3 digitalis glycosides
4.3.7.3.1 increased risk of arrhythmias
4.3.7.4 Lithium
4.3.7.4.1 increased plasma levels to Lithium
4.3.7.5 Propranolol
4.3.7.5.1 increased levels of Propranolol
4.3.7.6 Sulfonylureas
4.3.7.6.1 hyperglycemia
4.3.7.7 NSAIDs
4.3.7.7.1 blunted diuretic response
4.3.7.8 Probenecid
4.3.7.8.1 blunted diuretic response
4.3.7.9 Thiazide diuretics
4.3.7.9.1 synergy can lead to profound diuresis
4.3.7.10 Amphotericin B
4.3.7.10.1 increased chance of ototoxicity
4.3.8 Uses
4.3.8.1
4.3.8.1.1 Acute pulmonary edema
4.3.8.2
4.3.8.2.1 chronic congestive heart failure
4.3.8.3
4.3.8.3.1 hypertension
4.3.8.4
4.3.8.4.1 nephrotic syndrome
4.3.8.4.1.1 often unresponsive to other classes of diuretics
4.3.8.5
4.3.8.5.1 liver cirrhosis
4.3.8.5.1.1 to treat
4.3.8.5.1.1.1 edema
4.3.8.5.1.1.2 ascites
4.3.8.5.1.1.3 use with care
4.3.8.5.1.1.4
4.3.8.6
4.3.8.6.1 hypercalcemia
4.3.8.6.1.1 combine with isotonic saline to prevent fluid loss
4.3.8.7
4.3.8.7.1 some drug overdose
4.3.8.7.1.1 to induce forced diuresis
4.4 Thiazides
4.4.1 Examples
4.4.1.1 Hydrochlorothiazide
4.4.1.1.1 Ridaq
4.4.1.1.1.1
4.4.1.1.2 Hexazide
4.4.1.1.2.1
4.4.1.2 sulphonamides with thiazide effects
4.4.1.2.1 Chlorthalidone
4.4.1.2.1.1 Hygroton
4.4.1.2.2 Indapamide
4.4.1.2.2.1 Natrilix
4.4.1.2.2.1.1
4.4.1.2.2.2 Dapamax
4.4.1.2.2.2.1
4.4.1.2.2.3 Hydroless
4.4.1.2.2.3.1
4.4.1.2.3 Metolazone
4.4.1.2.3.1 Zaroxolyn
4.4.2 Mode of Action
4.4.2.1 inhibit Na+Cl- symport in DCT
4.4.2.1.1 increases Na+Cl- excretion
4.4.2.2 only moderately effective
4.4.2.2.1 90% of filtered sodium is reabsorbed before reaching the DCT
4.4.2.3 Increases K+ excretion
4.4.2.3.1 by sodium channels
4.4.2.4 chronic administration
4.4.2.4.1 increased uric acid levels
4.4.2.4.1.1 due to
4.4.2.4.1.1.1 increased reabsorbtion of uric acid
4.4.2.4.1.1.2 competition between diuretic and uric acid
4.4.2.4.1.1.2.1 for organic acid secretion in proximal tubule
4.4.2.4.1.1.2.1.1 reduced uric acid secretion
4.4.2.4.2 decrease Ca2+ excretion
4.4.2.4.2.1 can be used to treat kidney stones caused by hypercalciuria
4.4.2.4.3 can cause magnesium deficiency
4.4.2.5 do not alter kidney's ability to concentrate urine
4.4.2.6 effects on renal haemodynamics
4.4.2.6.1 do not effect RBF
4.4.2.6.2 do not effect TGF
4.4.2.6.2.1 thiazides act on a point past the macula densa
4.4.3 Adverse effects
4.4.3.1 rarely
4.4.3.1.1 CNS effects
4.4.3.1.1.1
4.4.3.1.1.1.1 vertigo
4.4.3.1.1.2
4.4.3.1.1.2.1 headache
4.4.3.1.1.3
4.4.3.1.1.3.1 paresthesias
4.4.3.1.1.3.1.1 Def: abnormal sensation of burning/prickling
4.4.3.1.1.4
4.4.3.1.1.4.1 weakness
4.4.3.1.2 gastrointestinal
4.4.3.1.2.1
4.4.3.1.2.1.1 anorexia
4.4.3.1.2.2
4.4.3.1.2.2.1 pancreatitis
4.4.3.1.2.3
4.4.3.1.2.3.1 nausea
4.4.3.1.2.3.2 vomiting
4.4.3.1.3 haematological
4.4.3.1.3.1
4.4.3.1.3.1.1 blood dyscrasias
4.4.3.1.3.1.1.1 Def: disorder of the cellular components of the blood
4.4.3.1.4
4.4.3.1.4.1 patients hypersensitive to sulphonamides
4.4.3.1.4.1.1 can cause
4.4.3.1.4.1.1.1 bone marrow depletion
4.4.3.1.4.1.1.2 skin toxicity
4.4.3.1.4.1.1.3 allergic reactions
4.4.3.1.4.1.1.4 photosensitivity
4.4.3.1.5
4.4.3.1.5.1 erectile dysfunction
4.4.3.1.5.1.1 greater than with other antihypertensive drugs
4.4.3.1.5.1.1.1 still tolerable
4.4.3.1.5.1.2 related to volume depletion
4.4.3.2 more serious
4.4.3.2.1
4.4.3.2.1.1 due to electrolyte and fluid imbalance caused
4.4.3.2.1.1.1 extracellular volume depletion
4.4.3.2.1.1.2 hypotension
4.4.3.2.1.1.3 hypochloremia
4.4.3.2.1.1.4 hypokalemic metabolic alkalosis
4.4.3.2.1.1.5 hypomagnesemia
4.4.3.2.1.1.6 hypercalcemia
4.4.3.2.1.1.7 hyponatremia
4.4.3.2.1.1.7.1 important
4.4.3.2.1.1.7.2 due to combination of
4.4.3.2.1.1.7.2.1 hypovolemia
4.4.3.2.1.1.7.2.1.1 causes increased level of ADH
4.4.3.2.1.1.7.2.1.1.1 reduction in diluting capacity of kidney
4.4.3.2.1.1.7.2.1.1.2 increased thirst
4.4.3.2.1.1.8 impaired carbohydrate tolerance
4.4.3.2.1.1.8.1 can cause hyperglycemia
4.4.3.2.1.1.9 hyperuricemia
4.4.3.2.1.1.10 hyperlipidemia
4.4.3.2.1.1.10.1 5-15% increase in
4.4.3.2.1.1.10.1.1 total serum cholesterol
4.4.3.2.1.1.10.1.2 LDL
4.4.4 Interactions
4.4.4.1 effects
4.4.4.1.1 anticoagulants
4.4.4.1.2 uricosuric agents
4.4.4.1.3 sulfonylureas
4.4.4.1.4 insulin
4.4.4.2 effects
4.4.4.2.1 anesthetics
4.4.4.2.2 Diazoxide
4.4.4.2.3 digitalis glycosides
4.4.4.2.4 lithium
4.4.4.2.5 loop diuretics
4.4.4.2.6 vitamin D
4.4.4.3 their effectiveness can be reduced by
4.4.4.3.1 NSAIDs
4.4.4.3.2 bile acid sequestrants
4.4.4.4 increased risk of hypokalemia
4.4.4.4.1 Amphotericin B
4.4.4.4.2 corticosteroids
4.4.4.5 torades du pointes
4.4.4.5.1 increased risk if given with Quinidine
4.4.4.5.2 increased risk factor potassium depletion
4.4.5 Uses
4.4.5.1
4.4.5.1.1 edema
4.4.5.1.1.1 due to
4.4.5.1.1.1.1
4.4.5.1.1.1.1.1 liver
4.4.5.1.1.1.1.1.1 cirrhosis
4.4.5.1.1.1.2
4.4.5.1.1.1.2.1 renal
4.4.5.1.1.1.2.1.1 nephrotic syndrome
4.4.5.1.1.1.2.1.2 chronic renal failure
4.4.5.1.1.1.2.1.3 acute glomerulonephritis
4.4.5.1.1.1.3
4.4.5.1.1.1.3.1 heart
4.4.5.1.1.1.3.1.1 congestive heart failure
4.4.5.2
4.4.5.2.1 hypertension
4.4.5.2.1.1 have additive and synergistic effects
4.4.5.2.1.1.1 when combined with other hypertensive agents
4.4.5.2.1.2 use only low doses
4.4.5.2.1.2.1 HCT 25mg per day
4.4.5.3
4.4.5.3.1 good choice
4.4.5.3.1.1 few contraindications
4.4.5.3.1.2 once daily dose
4.4.5.3.1.3 do not require dose titration
4.4.5.4
4.4.5.4.1 reduced calcium excretion
4.4.5.4.1.1 to treat kidney stones
4.4.5.4.1.2 to treat osteoporosis
4.4.5.5
4.4.5.5.1 nephrogenic diabetes insipidis
4.5 Potassium sparing diuretics
4.5.1 inhibitors of sodium channels
4.5.1.1 Examples
4.5.1.1.1 Triamterene
4.5.1.1.1.1 Dyazide
4.5.1.1.2 Amiloride
4.5.1.1.2.1 No single ingredient drug
4.5.1.1.2.1.1 Subtopic
4.5.1.2 Mode of Action
4.5.1.2.1 acts on collecting tubules and ducts
4.5.1.2.1.1 inhibits Na+ reabsorbtion and K+excretion
4.5.1.2.1.2 Amiloride blocks luminal sodium channels
4.5.1.2.1.2.1 by which Aldosterone produces its main effect
4.5.1.2.1.3 also has a Mg2+ sparing effect
4.5.1.2.1.4 both have mild uricosuric effect
4.5.1.3 Pharmacokinetics
4.5.1.3.1 Triamterene
4.5.1.3.1.1 rapid but incomplete oral absorption
4.5.1.3.1.1.1 30-70%
4.5.1.3.1.2 67% protein bound
4.5.1.3.1.3 half-life 1.5-2.5 hrs
4.5.1.3.1.3.1 diuretic effect
4.5.1.3.1.3.1.1 starts 2-4 hrs
4.5.1.3.1.3.1.2 lasts 7-9 hrs
4.5.1.3.1.4 elimination
4.5.1.3.1.4.1 extensive hepatic metabolism
4.5.1.3.1.4.1.1 mainly in faeces and bile
4.5.1.3.2 Amiloride
4.5.1.3.2.1 poor oral absorption
4.5.1.3.2.1.1 15-50%
4.5.1.3.2.2 minimal protein bound
4.5.1.3.2.3 half-life 6-9 hrs
4.5.1.3.2.4 elimination
4.5.1.3.2.4.1 unchanged in urine and faeces
4.5.1.4 Uses
4.5.1.4.1 usually in combination with other diuretics
4.5.1.4.2 where potassium sparing effect is required
4.5.1.4.2.1 hypertension
4.5.1.4.2.2 oedema
4.5.1.5 Adverse effects
4.5.1.5.1
4.5.1.5.1.1 hyperkalemia
4.5.1.5.1.1.1 mostly
4.5.1.5.2
4.5.1.5.2.1 skin rashes
4.5.1.5.3 less often
4.5.1.5.3.1
4.5.1.5.3.1.1 nausea
4.5.1.5.3.2
4.5.1.5.3.2.1 anorexia
4.5.1.5.3.3
4.5.1.5.3.3.1 abdominal pain
4.5.1.5.3.4
4.5.1.5.3.4.1 flatulance
4.5.1.5.3.5 Triampterene
4.5.1.5.3.5.1 poorly soluble in water
4.5.1.5.3.5.2 may precipitate in urine
4.5.1.5.3.5.2.1 cause kidney stones
4.5.1.5.3.5.2.1.1 drink plenty of water
4.5.2 Aldosterone antagonists
4.5.2.1 Examples
4.5.2.1.1 Spironolactone
4.5.2.1.1.1 Aldactone
4.5.2.1.1.1.1
4.5.2.1.1.2 Spiractin
4.5.2.1.1.2.1
4.5.2.2 Mode of Action
4.5.2.2.1
4.5.2.2.1.1 metabolised in liver
4.5.2.2.1.1.1 to active metabolite
4.5.2.2.1.1.1.1 canrenone
4.5.2.2.1.1.1.1.1 also an antagonist of aldosterone
4.5.2.2.2
4.5.2.2.2.1 aldosterone receptors
4.5.2.2.2.1.1 in distal tubule
4.5.2.2.2.1.1.1 only diuretic that acts on
blood side of tubule
4.5.2.2.2.1.2 and collecting duct
4.5.2.2.2.1.3 antagonist
4.5.2.2.2.1.3.1 competes with aldosterone for
intracellular aldosterone receptors
4.5.2.2.2.1.3.1.1 this complex inhibits the sodium retaining action of aldosterone
4.5.2.2.2.1.3.1.1.1 also causes concomitant decreae in potassium secretion
4.5.2.2.2.1.3.1.2 Figure of action
4.5.2.2.2.1.3.1.2.1
4.5.2.2.3
4.5.2.2.3.1 has some affinity for progesterone and androgen receptors
4.5.2.2.3.1.1 causes side effects
4.5.2.2.3.1.1.1 see below
4.5.2.2.4
4.5.2.2.4.1 renal hemodynamics
4.5.2.2.4.1.1 no effects
4.5.2.3 Pharmacokinetics
4.5.2.3.1
4.5.2.3.1.1 orally
4.5.2.3.1.1.1 well absorbed
4.5.2.3.2
4.5.2.3.2.1 protein bound
4.5.2.3.2.1.1 highly
4.5.2.3.3
4.5.2.3.3.1 liver
4.5.2.3.3.1.1 25 - 30% metabolised to canrenone
4.5.2.3.3.1.1.1 half-life of 13-24 hrs
4.5.2.3.4
4.5.2.3.4.1 elimination
4.5.2.3.4.1.1 mostly renal
4.5.2.3.5
4.5.2.3.5.1 half-life short 1.6 hrs
4.5.2.3.5.1.1 canrenone long (see above)
4.5.2.3.6
4.5.2.3.6.1 high concentrations
4.5.2.3.6.1.1 can inhibit
4.5.2.3.6.1.1.1 cytochrome P450 steroid hydroxylase
4.5.2.3.7 uses
4.5.2.3.7.1 mostly in cases of mineralocorticoid excess
4.5.2.3.7.1.1 due to
4.5.2.3.7.1.1.1 hypersecretion
4.5.2.3.7.1.1.2 aldosteronism
4.5.2.3.7.1.1.2.1 due to
4.5.2.3.7.1.1.2.1.1 chronic heart failure
4.5.2.3.7.1.1.2.1.2 hepatic cirrhosis
4.5.2.3.7.1.1.2.1.3 nephrotic syndrome
4.5.2.3.7.2 in combination with loop and thiazide diuretics
4.5.2.3.7.2.1 to limit potassium loss
4.5.2.3.7.2.1.1 esp where hypokalemia is dangerous
4.5.2.3.7.2.1.1.1 patients on digitalis
4.5.2.4 Adverse effects
4.5.2.4.1 frequent
4.5.2.4.1.1
4.5.2.4.1.1.1 hyperkalemia
4.5.2.4.1.1.1.1 where potassium excretion is reduced
4.5.2.4.1.1.1.1.1 risk is increased in renal disease
4.5.2.4.1.1.1.1.2 drugs
4.5.2.4.1.1.1.1.2.1 that reduce renin
4.5.2.4.1.1.1.1.2.1.1 NSAIDs
4.5.2.4.1.1.1.1.2.1.2 beta-blockers
4.5.2.4.1.1.1.1.2.2 reduce angiotensin activity
4.5.2.4.1.1.1.1.2.2.1 ACE inhibitors
4.5.2.4.1.1.1.1.2.2.2 angiotensin receptor inhibitors
4.5.2.4.2 less frequent
4.5.2.4.2.1
4.5.2.4.2.1.1 hyponaturemia
4.5.2.4.2.2
4.5.2.4.2.2.1 dehydration
4.5.2.4.2.3
4.5.2.4.2.3.1 oestrogen-like effects
4.5.2.4.2.3.1.1
4.5.2.4.2.3.1.1.1 gynocomastia
4.5.2.4.2.3.1.2
4.5.2.4.2.3.1.2.1 decreased libido
4.5.2.4.2.3.1.3
4.5.2.4.2.3.1.3.1 impotence
4.5.2.4.2.3.1.4
4.5.2.4.2.3.1.4.1 benign prostatic hyperplasia
4.5.2.4.2.3.1.5
4.5.2.4.2.3.1.5.1 menstrual irregularities
4.5.2.4.2.3.1.6
4.5.2.4.2.3.1.6.1 postmenopausal bleeding
4.5.2.4.2.3.1.7
4.5.2.4.2.3.1.7.1 hirsutism
4.5.2.4.2.4
4.5.2.4.2.4.1 gastric effects
4.5.2.4.2.4.1.1
4.5.2.4.2.4.1.1.1 diarrhoea
4.5.2.4.2.4.1.2
4.5.2.4.2.4.1.2.1 gastritis
4.5.2.4.2.4.1.3
4.5.2.4.2.4.1.3.1 gastric bleeding and peptic ulcers
4.5.2.4.2.4.1.3.1.1 contraindicated in people with ulcers
4.5.2.4.2.5
4.5.2.4.2.5.1 CNS effects
4.5.2.4.2.5.1.1
4.5.2.4.2.5.1.1.1 drowsiness
4.5.2.4.2.5.1.2
4.5.2.4.2.5.1.2.1 lethargy
4.5.2.4.2.5.1.3
4.5.2.4.2.5.1.3.1 ataxia
4.5.2.4.2.5.1.3.1.1 DEF: failure of muscular coordination
4.5.2.4.2.5.1.4
4.5.2.4.2.5.1.4.1 confusion
4.5.2.4.2.5.1.5
4.5.2.4.2.5.1.5.1 headache
4.5.2.4.2.6
4.5.2.4.2.6.1 in cirrhotic patients
4.5.2.4.2.6.1.1 can induce metabolic acidosis
4.5.2.4.2.6.1.1.1 by inhibiting H+ secretion
4.5.2.4.3 has advantage of not effecting
4.5.2.4.3.1
4.5.2.4.3.1.1 glucose metabolism
4.5.2.4.3.2
4.5.2.4.3.2.1 uric acid elimination
|
| |